How Healthcare Providers Are Preparing for the New Age of Pricing Transparency in 2019
Roundtable Recap
Price Transparency Roundtable Recap
PMMC hosted a roundtable interview with four Revenue Cycle experts from healthcare providers across the country.
The panelists were asked a series of questions and shared unique insight into how healthcare providers responded to the CMS Price Transparency Final Rule as well as concerns and opportunities in today's new age of price transparency.
Read panelist responses below:
What is your hospital's biggest concern now that standard charges are public?
How do you see price transparency affecting your hospital's charges?
How do you see price transparency affecting competition in your market and how are you responding to it?
What do you think will be the next set of CMS price transparency requirements?
What do you think will be the biggest impact of price transparency in the next two to three years?
Meet the Panelists
 Susan Downey, Manager of Pricing & CDM, Virginia Mason Medical Center
Susan Downey, Manager of Pricing & CDM, Virginia Mason Medical Center
Susan has eighteen years of experience with healthcare pricing in both the hospital realm and in health insurance. Susan is excited about the opportunity to educate patients regarding the true cost of care. With the ever-changing landscape of healthcare, particularly with the current emphasis on transparency, she expects this to be a fulfilling challenge. Susan holds an MBA in Healthcare Management from Western Governors University and a BS in Actuarial Science from Central WA University.
 Kabby Thompson, Director of Managed Care, Texas Children's Hospital
Kabby Thompson, Director of Managed Care, Texas Children's Hospital
Kabby is currently the Director of Managed Care for Texas Children’s Hospital System. She has over 20 years of experience in managed care contracting for both managed care organizations. Prior to Texas Children’s Kabby worked for BCBSTX. She has extensive experience negotiating in a highly complex and competitive market with hospital systems, large physician groups and ancillary providers. Kabby’s experience has also included managing specialty network development for Centers of Excellence programs and more recently the implementation of Value-Based Contracts.
How did your organization respond to the CMS price transparency final rule to electronically post your standard list of prices?
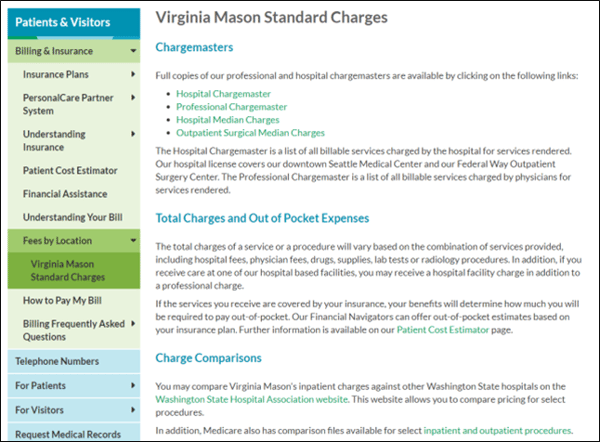
Susan Downey, Virginia Mason Medical Center:
We developed a webpage specifically to address this regulation. We already had files available due to the current ACA regulation, they simply needed to be converted to a machine readable format. Since our organization is an integrated health system, we published both our hospital and professional Chargemaster’s based on the feedback we heard during the Open Door Forums.
For the DRG file, we choose to use the median charge. In addition, we decided to publish our outpatient surgical median charges as well.
Additionally, the webpage directs the patient on how to obtain an out of pocket estimate and financial assistance. There is a link to email the Chargemaster Department with questions.
Kabby Thompson, Texas Children's Hospital:
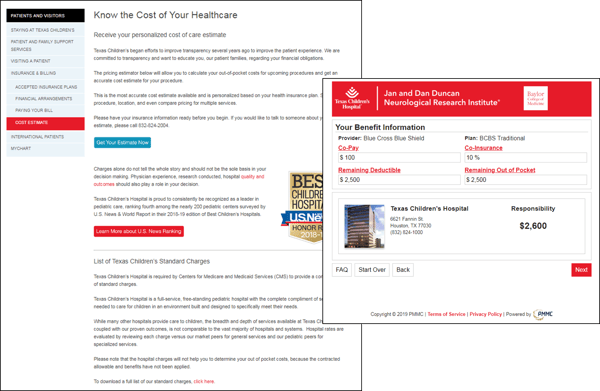
We chose to expand upon our current practice of providing patient estimates prior to the date of service with a self-estimate tool online in addition to information that helps to explain why children’s hospitals cannot be compared to general hospitals and links to our quality data.
We could not have done this without the help and dedication of PMMC, who was committed to helping us meet our deadline for January 1.
Greg Kay, PMMC:
From a broader industry perspective, PMMC’s research of single hospitals and multi-facility healthcare systems found that 87% of the hospitals have met the CMS requirement to post a list of standard charges with the data being relatively easy to find (5 clicks or less).
We also found that 38% provided the required list of prices by DRG code and 88% of the files that were posted online appeared to include Pharmacy.
Going beyond CMS’ requirement and being proactive, the survey also found 86% included a phone number to contact for more information and 10% actually have an online consumer estimate pricing tool.
Through our market research, we also identified several items that we thought were noteworthy as best practices. A common theme that we saw tied to Chargemaster files was educational information explaining the role of charges, the payer allowable, what the patient owes as well as disclaimer forms. This helps reinforce and support your hospital’s pricing message. As an example it should call out key points such as the hospital provides price estimates for many "common services" with a phone number to call for an estimate.
A more creative example we found was a 90 second video that explained the difference between charges and out-of-pocket costs. This hospital requires the patient to watch the entire video before allowing them to access their charge file.
We thought this was a great way to educate the patient.
Brad Josephson, PMMC:
In our market research, we found that most hospitals posted their CDM in an Excel or CSV file, but we found a few instances of a Text file. I would argue this is harder to read and makes it more difficult for the patient to consume the information.
We also evaluated what was included in the Chargemaster file itself. We found that of the 87% of hospitals that did post their chargemaster, they all included both the charge description and the price.
While posting this information in a machine readable format meets the mandate, it’s worth pointing out that if a patient really wanted to compare charges at different hospitals, the CPT code would be the most valuable identifier. In this case, we found that only 14% of hospitals included the CPT Code.This could also be due to hospital not wanting to make it too easy for competitors to compare charges.
What is your hospital's biggest concern now that standard charges are public?
Kabby Thompson, Texas Children's Hospital:
The biggest concern is misinterpretation of the chargemaster by patients, who might think that this is their out of pocket expense.
Brad Josephson, PMMC:
Adding to the concerns about public misperception, we have already seen a good amount of media coverage since the mandate both on the national and local level.
National outlets, like CNN and Modern Healthcare, were somewhat critical of the information being posted. Modern Healthcare took it a step further by calling out specific hospitals that did not do a good job of displaying the chargemaster information. This was the type of response that I think a lot of us were concerned about.
Perhaps more impactful for individual hospitals today is the local media coverage.
I’ve seen several articles posted on social media that call into question some of the higher priced commodity items and we all know how easily and quickly that information is shared now on platforms like Facebook and Twitter.
A news outlet in Louisville, Kentucky compared the four major hospital groups in the market and focused on the large pricing discrepancy on some procedures and treatments.
This is something that is very preventable and manageable by simply doing a local charge comparison to make sure charges are in line with the market.
How do you see price transparency affecting your hospitals charges?
Susan Downey, Virginia Mason Medical Center:
I don’t see it impacting how we currently set rates. We already use market data, in addition to cost and contract rates. Our pricing is competitive with the market. Unless there is a big shift in the market, we will not make any big changes.
Kabby Thompson, Texas Children's:
I don’t think that merely posting a chargemaster will prompt change in the industry. Making changes to pricing or chargemaster prices, will not change the true cost of healthcare. Nor will it help average consumers to understand their costs. It will only lead to more confusion. The chargemaster is merely a symptom of larger problems that cannot be fixed overnight. They require a long term evolution of change.
How do you see price transparency affecting competition in your market and how are you responding to it?
Susan Downey, Virginia Mason Medical Center:
I do not believe simply having everyone publish their chargemaster will impact competition. Most patients will not understand the chargemaster.
Until there is a tool that can accurately compare a procedure across multiple organizations, this information is of no help to patients.
We have a tool that allows patients to get an estimate of their actual out of pocket costs for their procedure. Since we are an integrated system, this includes all charges – professional and facility. This type of information is where the industry needs to go.
What do you think will be the next set of CMS price transparency requirements?
Greg Kay, PMMC:
In looking back over the past six months of interviews and the frequently asked questions responses that CMS has published, I believe they have been very clear with their direction. They expect the industry to lead this transformation and not wait for CMS to dictate steps forward.
CMS has been very clear and Seema Verma continues to reinforce the message that posting charges is the first step. Their goal and their intent of these requirements is to make pricing transparency actionable.
Nearly 21 Million Americans had a HDHP or HSA in 2017 and this number will continue to rise. Their financial responsibility is tied to their insurance carrier’s allowable, their co-pay, co-insurance, deductible and remaining out of pocket. CMS’ requirement to post charges is seen as a means of increasing competition which is viewed as increasing affordability. There is large variability in charges and reimbursement.
The expectation is that our historical patient who went where they were told when there was little financial personal investment will start to make decisions with their wallet when they better understand the real cost of care.
As an example, CMS’ intention is not only to increase pricing transparency but actually be the catalyst for a new means of shopping for healthcare. Last year, CMS deployed a new Procedure Price Lookup tool.
Keep in mind, it is a very simple tool at this stage. Users can search by procedure name or code. Over time, this tool will become easier and smarter.
Once a code is selected, the user can see the average Medicare beneficiary’s financial responsibility if that procedure occurs in an ASC setting or in a hospital outpatient department. CMS’ goal is to provide insightful pricing information so patients can make better decisions for their healthcare and their wallet. In this particular example, patients will now be able to see the average cost difference. This will likely lead to more detailed questions from patients going forward.
We anticipate future versions will be hospital specific and not just an average.
CMS expects our industry to have leaders that will lead -- we do not have to wait. We absolutely must move to helping patients understand what the cost of care will be for them.
Looking further out in time with some historical perspective, CMS’ requirement for more pricing transparency ties to their migration with bundled payments, shared saving arrangements and value-based contracts.
As a target, we need to be moving to provide our patients with an estimate for a true cost of care. To those electing not to move this direction, please recognize that others are and they will be the ones controlling the price message and where patients go for care.
What do you think will be the biggest impact that price transparency will have on the health care industry in the next two to three years?
Susan Downey, Virginia Mason Medical Center:
Hopefully it will push the conversation. Financial health is as important for a patient as physical health. Currently, the tools for the patient to use to assist in decision making do not exist on a broad spectrum. Individual facilities can provide information, but only for the services they provide. It is up to the patient to track down all of the different information and they do not have a complete understanding of the system. While I do not believe publishing the chargemaster is helpful, it at least gets things started.
___________________________________________
 Susan Downey, Manager of Pricing & CDM, Virginia Mason Medical Center
Susan Downey, Manager of Pricing & CDM, Virginia Mason Medical Center Kabby Thompson, Director of Managed Care, Texas Children's Hospital
Kabby Thompson, Director of Managed Care, Texas Children's Hospital